Summary: By using better masks, monitoring and improving indoor air quality, and rolling out rapid tests, we could quickly halt the current outbreaks in the Australian states of New South Wales (NSW) and Victoria. If we fail to do so, and open up before 80% of all Australians are vaccinated, we may have tens of thousands of deaths, and hundreds of thousands of children with chronic illness which could last for years.
We can get R under 1.0
Pandemics either grow exponentially, or disappear exponentially. They don’t just stay at some constant level. If the reproduction number R, which is how many people each infected person transmits to, is greater than 1.0 in a region, then the pandemic grows exponentially and becomes out of control (as we see in NSW now), or it is less than 1.0, in which case the virus dies out.
No Australian state or territory is currently using any of the three best “bang for your buck” public health interventions: better masks, better ventilation, or rapid testing. Any of these on their own (combined with the existing measures being used in Vic) would likely be enough to get R<1. The combination of them would probably kill off the outbreaks rapidly. At that point life can largely return to normal.
Stopping delta is not impossible. Other jurisdictions have done it, including Taiwan and China. New Zealand appears to be well on the way too. There’s no reason Australia can’t join them.
Better masks
Scientists have found that using better masks is the single best way to decrease viral transmission in a close indoor setting. They showed that if all teachers and students wear masks with good fit and filtration, transmission is reduced by a factor of around 300 times. The CDC has found that two free and simple techniques to enhance the fit of surgical masks, “double masking” and “knot and tuck”, both decrease virus exposure by a factor of more than ten compared to wearing a cloth or surgical mask alone. For more information, see my article (with Zeynep Tufekci) in The Atlantic.
Ventilation
We now know that covid is airborne. That means that we need clean air. A recent study has shown that the key to managing this is to monitor CO2 levels in indoor spaces. That’s because CO2 levels are a good proxy for how well air is being circulated. Without proper ventilation, CO2 levels go up, and if there are infected people around virus levels go up too.
CO2 monitors can be bought in bulk for around $50. Standards should be communicated for what acceptable maximum levels of CO2 are for classrooms, workplaces, and public indoor spaces, and education provided on how to improve air quality. Where CO2 levels can not be controlled, air purifiers with HEPA filtration should be required.
Better ventilation can decrease the probability of infection by a factor of 5-10 compared to indoor spaces which do not have good airflow.
Rapid tests
Rapid antigen lateral flow tests are cheap, and provide testing results within 15-30 minutes. They have very few false positives. A Brisbane-based company, Ellume, has an FDA approved rapid test, and is exporting it around the world. But we’re not using it here in Australia.
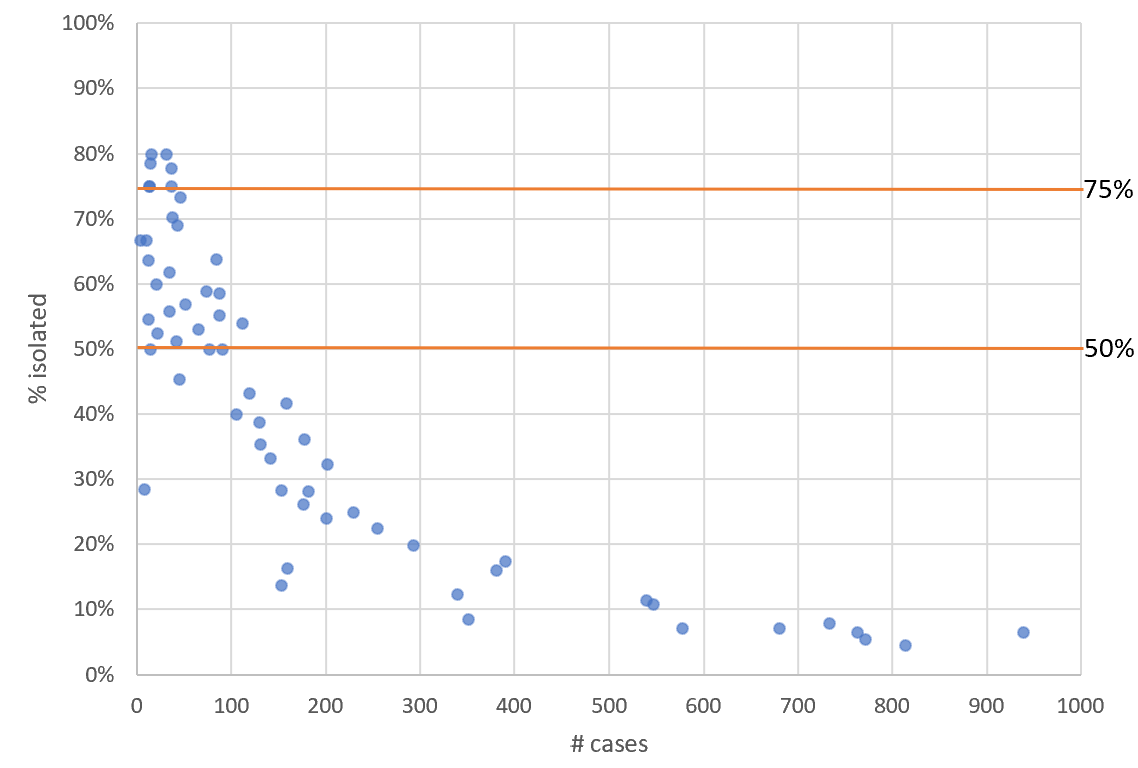
If every workplace and school required daily rapid tests, around 75% of cases in these locations would be identified. Positive cases would isolate until they have results from a follow-up PCR test. Using this approach, transmission in schools and workplaces would be slashed by nearly three quarters, bringing R well under 1.0.
In the UK every child was tested twice a week in the last school term. Recent research suggests that daily rapid tests could allow more students to stay at school.
Hitting a vaccination target
The Grattan Institute found we need to vaccinate at least 80% of the total population (including children) this year, and continue the vaccination rollout to 90% throughout 2022. Clinical trials for the vaccine in kids are finishing this month. If we can quickly ramp up the roll-out to kids, and maintain the existing momentum of vaccinations in adults, we may be able to achieve the 80% goal by the end of the year.
It’s important to understand, however, that no single intervention (including vaccination) will control covid. Many countries with high vaccination rates today have high covid death rates, due to waning immunity and unvaccinated groups. The point of all of these interventions is to reduce R. When R is under 1 and cases are under control, restrictions are not needed; otherwise, they are needed.
We must get R under 1.0
Over 200,000 children will develop chronic illness
The Doherty Report predicts that over three hundred thousand children will get symptomatic covid, and over 1.4 million kids will be infected, in the next 6 months if restrictions are reduced when 70% of adults are vaccinated. This may be a significant under-estimate: a recent CDC study predicts that 75% of school-kids would get infected in three months in the absence of vaccines and masks.
New research has found that one in seven infected kids may go on to develop “long covid”, a debilitating illness which can impact patients for years. Based on this data, we are looking at two hundred thousand kids (or possibly far more) with chronic illness. The reality may be even worse than this, since that research uses PCR tests to find infected kids, but PCR testing strategies have been shown to fail to identify covid in kids about half the time. Furthermore, this study looked at the alpha variant. The delta variant appears to be about twice as severe.
It’s too early to say when, or if, these children will recover. Some viruses such as polio led to life-long conditions, which weren’t discovered until years later. Long covid has a lot of similarities to myalgic encephalomyelitis, which for many people is a completely debilitating life-long condition.
In regions which have opened up, such as Florida, schools were “drowning” in cases within one week of starting term. In the UK, lawsuits are now being filed based on the risks being placed on children.
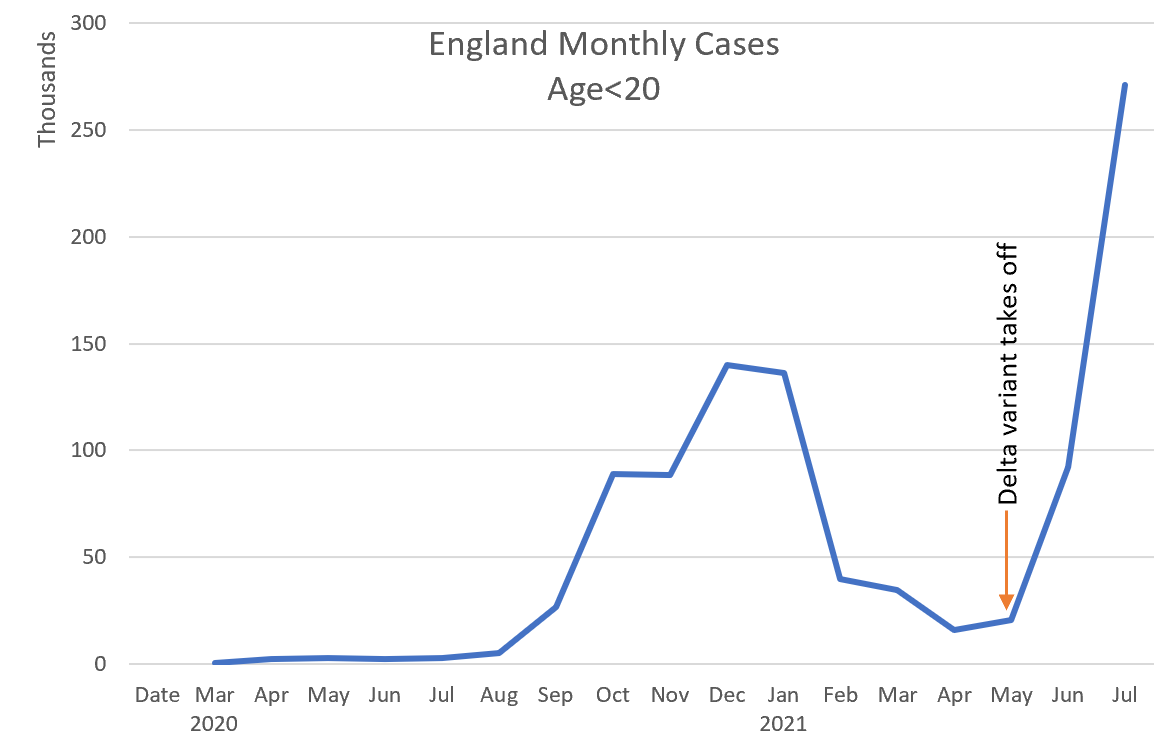
Delta rips through unvaccinated populations. For instance, in England delta took hold during May 2021. English schools took a cautious approach, placing school children in “bubbles” which did not mix. After school children were required to go directly home and not mix with anyone else. Nonetheless, within three months, more kids were getting infected than had ever been before. Cases in July 2021 were around double the previous worst month of December 2020.
The Doherty Model greatly underestimates risks
The Doherty Model, which is being used as a foundation for Australian reopening policy, has many modeling and reporting issues which result in the Doherty Report greatly underestimating risks. (These issues are generally a result of how the report was commissioned, rather than being mistakes made by those doing the modeling.)
The Doherty Model has to work with incomplete data, such as the very limited information we have about the behavior of the delta variant. The recommended practice in this kind of situation is to not make a single assumption about the premises in a model, but to instead model uncertainty, by including a range of possible values for each uncertain premise. The Doherty Model does not do this. Instead, “point estimates”, that is, a single guess for each premise, are used. And a single output is produced by the model for each scenario.
This is a critical deficiency. By failing to account for uncertainty in inputs, or uncertainty in future changes (such as new variants), the model also fails to account for uncertainty in outputs. What’s the probability that the hospitalizations are far more rapid than in their single modeled outcome, such that Australian ICUs are overloaded? We don’t know, because that work hasn’t been done.
The Doherty Model makes a critical error in how it handles the Delta variant: “we will assume that the severity of Delta strains approximates Alpha strains”. We now know that it is incorrect: latest estimates are that “People who are infected with the highly contagious Delta variant are twice as likely to be hospitalized as those who are infected with the Alpha variant”.
The model also fails to correctly estimate the efficacy of Test, Trace, Isolate, and Quarantine (TTIQ). It assumes that TTIQ will be “optimal” for “hundreds of daily cases”, and “partial” for thousands of cases. However, in NSW optimal TTIQ was no longer maintained after just 50 cases, and the majority of cases were no longer isolating after 100 daily cases.
The Doherty Model assumes that vaccines are equally distributed throughout the country. This is mentioned in the report, and has also been confirmed by talking directly with those doing the modeling. However, there are groups where that’s not true. For instance, indigenous communities are only around ⅛ vaccinated. In this group, if restrictions are removed, then R will return towards 5.0 (the reproduction number of delta without vaccines or restrictions). As a result, nearly the entire population will be infected within months.
The same thing will happen with kids. The Doherty model fails to model school mixing, but instead makes a simplifying assumption that children have some random chance of meeting random other children each day. In practice however, they have a 100% chance of mixing with exactly the same children every day, at school.
The Doherty Model misses the vast majority of cases. That’s because it entirely ignores all cases after 180 days (when most cases occur). Another model has estimated the full impact of covid without such a time limitation. It finds that there would be around 25,000 deaths in Australia in the absence of restrictions.
A major problem with the National Plan based on the Doherty Report is that it goes directly from vaccination rate to actions, and bakes in all the model assumptions. It can’t take into account unanticipated changes, such as more transmissible variants, or mass infections of hospital staff.
It would be far better to decide actions in terms of measurements that reflect changing current conditions — that is, R and remaining health-care Capacity. The Doherty Institute models could be reported as estimated R and Capacity at 70% and 80% vaccination rates of adults, which is 56% and 64% of the full population.
Reducing transmission restrictions when R>1 or there is insufficient remaining capacity would be madness regardless of the vaccination rate.
“Live with covid” means mass hospitalizations and ongoing outbreaks
Based on current projections, the best case scenario in one month’s time there will be over 2000 people hospitalized with covid in NSW, with over 350 in ICU. This is going to be a big stretch on the state’s resources. The same will happen in other states that fail to control outbreaks prior to achieving at least 80% vaccination rates of all populations, including children and indigenous communities.
Even when most adults are vaccinated, covid doesn’t go away. Immunity wanes after a few months, and there will continue to be groups where fewer people have been vaccinated. We can estimate the longer term impact of covid by looking at other countries. In the UK, 75% of 16+ residents are vaccinated. There are currently 700 covid deaths and 250,000 cases per week in the UK. If our death rate is proportionate, that would mean 266 Australians dying per week even after we get to 75% vaccinated (along with thousands of long covid cases, with their huge economic and societal cost). By comparison, there were 9 weekly deaths from flu in Australia in 2019.
Conclusion
We are now hearing political leaders in Victoria and NSW giving up on getting the outbreaks under control. But we haven’t yet deployed the three easiest high-impact public health interventions we have at our disposal: better masks, better ventilation, and rapid tests. Any one of these (along with the existing measures) would be likely to neutralize the outbreaks; their impacts combined will be a powerful weapon.
If we don’t do this, then covid will leave hundreds of thousands of Australian children with chronic illness, and kill thousands of Australians. This is entirely avoidable.
Acknowledgements: Thanks to Dr Rachel Thomas for many discussions about this topic and for draft review. Thanks also to the many Australian scientists with whom I consulted during development of this article.